In our interconnected world, understanding the landscape of global health threats has never been more crucial. While many focus on headline-grabbing pandemics, some of the most dangerous diseases in today’s society operate quietly, claiming millions of lives annually without making front-page news. Among these silent killers, lower respiratory tract infections stand as one of the most significant challenges facing global public health.
The Hidden Reality of Respiratory Infections
Lower respiratory tract infections represent a category of illnesses that affect the lungs and breathing passages below the voice box. These infections, which include pneumonia, bronchitis, and bronchiolitis, consistently rank among the top causes of mortality worldwide. According to the World Health Organization’s latest mortality statistics, these infections claim approximately 2.6 million lives annually, making them the fourth leading cause of death globally.
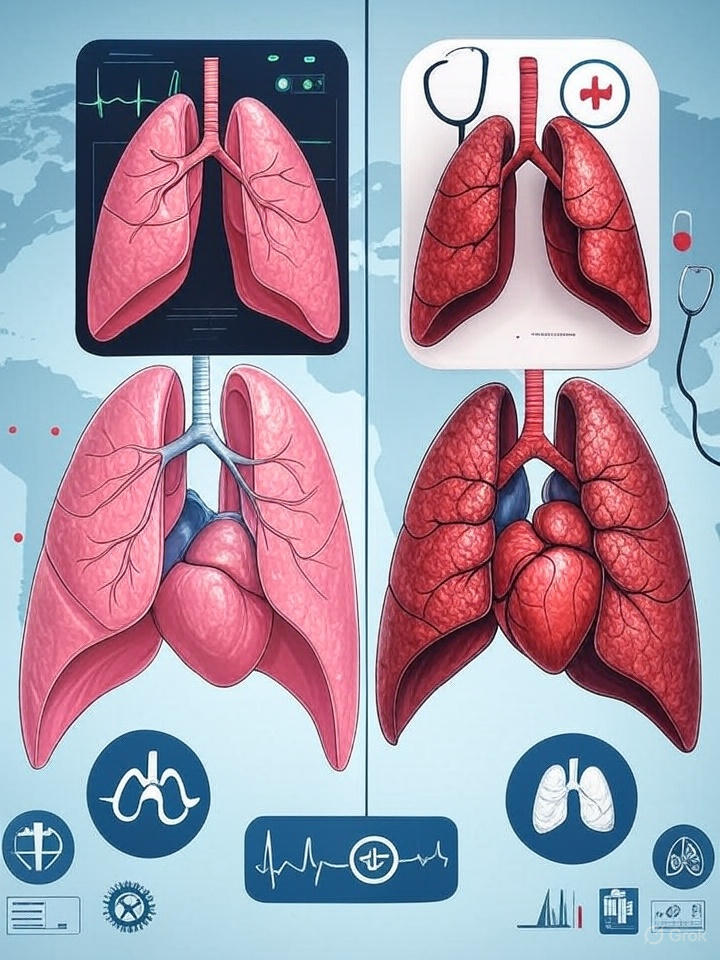
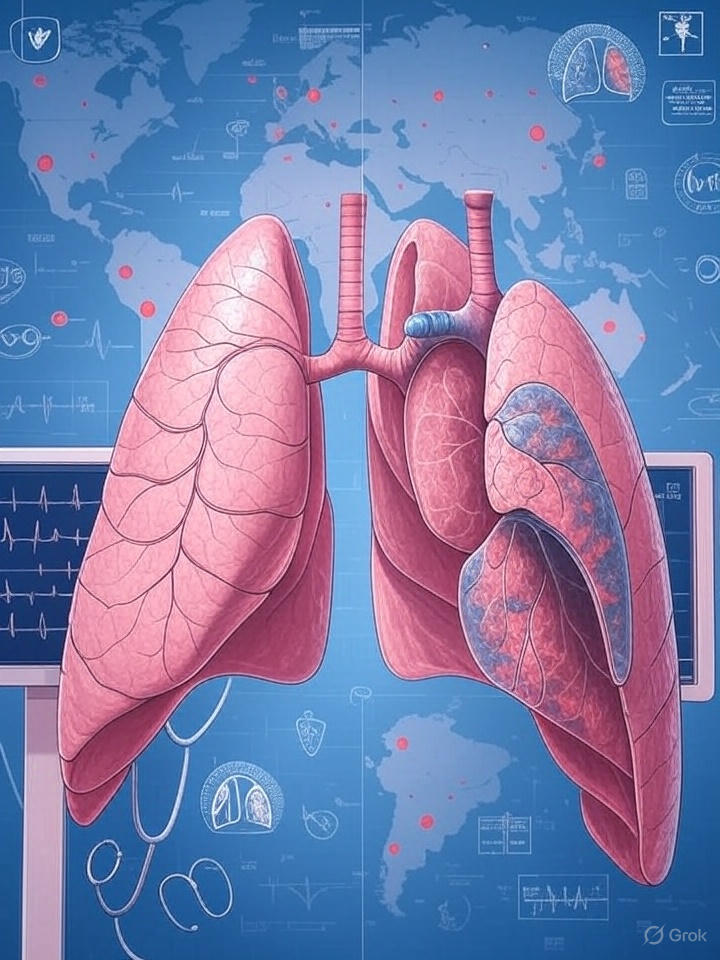
The term “lower respiratory tract infection” encompasses various conditions that affect the lungs’ delicate structures. Unlike upper respiratory infections such as common colds, these conditions penetrate deeper into the respiratory system, affecting the bronchi, bronchioles, and alveoli where crucial gas exchange occurs. This deeper penetration makes them significantly more dangerous and potentially life-threatening.
Understanding the Pathophysiology
The lower respiratory system consists of intricate networks of airways and air sacs designed for efficient oxygen exchange. When pathogens—whether bacterial, viral, or fungal—invade these structures, they trigger inflammatory responses that can severely compromise breathing function. The body’s natural defense mechanisms, including mucus production and immune cell activation, sometimes become overwhelmed, leading to the characteristic symptoms of lower respiratory tract infections.
Pneumonia, the most common and deadly form of lower respiratory tract infection, occurs when infection causes inflammation in the air sacs of one or both lungs. These air sacs may fill with fluid or pus, causing cough with phlegm, fever, chills, and difficulty breathing. The condition can range from mild to life-threatening, particularly affecting vulnerable populations such as infants, elderly individuals, and those with compromised immune systems.
Global Mortality Data: The Statistical Reality
Recent global mortality data from the World Health Organization reveals alarming trends in respiratory infection deaths. The burden of these diseases disproportionately affects low- and middle-income countries, where access to healthcare, proper nutrition, and sanitation remains limited. However, even developed nations face significant challenges from these infections, particularly among aging populations and individuals with chronic conditions.
The geographic distribution of lower respiratory tract infection deaths highlights stark health inequities. Sub-Saharan Africa and South Asia bear the heaviest burden, accounting for nearly 60% of global deaths from these conditions. This disparity reflects complex interactions between poverty, malnutrition, air pollution, and limited healthcare infrastructure.
Seasonal patterns also play crucial roles in mortality rates. Winter months typically see spikes in respiratory infections due to increased indoor crowding, reduced humidity, and compromised immune function. Climate change has begun altering these traditional patterns, with some regions experiencing prolonged seasons of increased transmission risk.
Age-Specific Vulnerabilities
Children under five years of age face particularly high risks from lower respiratory tract infections. Their developing immune systems, smaller airways, and higher breathing rates make them more susceptible to severe complications. Pneumonia alone kills more children worldwide than any other infectious disease, claiming the lives of over 700,000 children under five annually.
At the other end of the age spectrum, adults over 65 experience dramatically increased mortality rates from these infections. Age-related changes in immune function, the presence of chronic conditions, and physical frailty contribute to poorer outcomes. The case fatality rate for pneumonia in elderly populations can exceed 20%, making prevention and early treatment critical priorities.
Smoking-Related Lung Disease Statistics: A Preventable Crisis
The relationship between tobacco use and respiratory disease represents one of public health’s most documented and preventable tragedies. Smoking-related lung disease statistics from the Centers for Disease Control reveal that tobacco use contributes to approximately 480,000 deaths annually in the United States alone, with respiratory diseases accounting for a significant portion of these fatalities.
Chronic obstructive pulmonary disease (COPD), primarily caused by smoking, affects over 250 million people worldwide and ranks as the third leading cause of death globally. This progressive disease encompasses emphysema and chronic bronchitis, conditions that gradually destroy lung tissue and impair breathing function. The economic burden of COPD extends far beyond healthcare costs, affecting productivity, quality of life, and family financial stability.
The Mechanism of Tobacco-Induced Lung Damage
Cigarette smoke contains over 7,000 chemicals, with at least 70 known carcinogens. These substances trigger chronic inflammation in the respiratory tract, leading to structural changes that compromise lung function. The constant exposure to toxic compounds overwhelms the lungs’ natural cleaning mechanisms, allowing harmful particles and pathogens to accumulate.
The progression from healthy lungs to severely damaged respiratory systems follows predictable patterns. Initial exposure causes acute inflammatory responses, which, over time, lead to chronic inflammation, tissue remodeling, and irreversible damage. Former smokers can experience some recovery of lung function, but certain changes remain permanent, highlighting the importance of prevention over treatment.
Secondhand smoke exposure poses additional risks, particularly for children and non-smoking adults. The American Lung Association reports that secondhand smoke causes approximately 41,000 deaths annually among non-smoking adults and increases the risk of lower respiratory tract infections in children by 50-100%.
Ischemic Heart Disease: The Silent Epidemic
While respiratory infections capture attention for their acute nature, ischemic heart disease operates as a silent epidemic, claiming more lives than any other single condition worldwide. This cardiovascular condition, characterized by reduced blood flow to the heart muscle, represents the leading cause of death globally, responsible for approximately 9 million deaths annually.
The relationship between ischemic heart disease and respiratory health creates complex clinical scenarios. Patients with heart disease often develop secondary respiratory complications, while severe respiratory infections can trigger cardiac events. This interconnection highlights the importance of comprehensive healthcare approaches that address multiple organ systems simultaneously.
Understanding Coronary Artery Disease Symptoms
Coronary artery disease symptoms often develop gradually, making early detection challenging. The classic presentation includes chest pain or discomfort, particularly during physical activity or emotional stress. However, many patients experience atypical symptoms, including shortness of breath, fatigue, and pain in the neck, jaw, or back.
Women frequently present with different symptom patterns than men, often experiencing more subtle signs such as nausea, lightheadedness, or unusual fatigue. These gender differences in presentation can lead to delayed diagnosis and treatment, contributing to poorer outcomes in female patients.
The progression of coronary artery disease involves gradual narrowing of the arteries that supply blood to the heart muscle. This narrowing typically results from atherosclerosis, a process where fatty deposits accumulate in arterial walls. Over time, these deposits can rupture, triggering blood clot formation that can completely block blood flow, resulting in heart attacks.
Environmental Factors and Disease Prevention
The role of environmental factors in respiratory and cardiovascular disease cannot be overstated. Air pollution, both outdoor and indoor, contributes significantly to the global burden of respiratory infections and chronic diseases. The World Health Organization estimates that air pollution causes 7 million premature deaths annually, with respiratory and cardiovascular diseases accounting for the majority of these fatalities.
Indoor air pollution poses particular risks in developing countries where biomass fuels are commonly used for cooking and heating. Women and children face the highest exposure levels, spending significant time near cooking fires that produce harmful particulates and toxic gases. This exposure pattern explains, in part, the higher rates of respiratory infections among these populations.
Urban air pollution presents different challenges, with vehicle emissions, industrial activities, and power generation contributing to complex mixtures of harmful pollutants. Fine particulate matter (PM2.5) and ground-level ozone represent the most significant threats, capable of penetrating deep into lung tissue and entering the bloodstream.
Climate Change and Health Impacts
Climate change increasingly influences patterns of respiratory and cardiovascular disease through multiple pathways. Rising temperatures extend pollen seasons, worsen air quality, and create conditions favorable for infectious disease transmission. Extreme weather events disrupt healthcare systems and force population movements that can spread infections.
The Lancet Commission on Health and Climate Change identifies respiratory infections as among the health threats most sensitive to climate variability. Changes in temperature and precipitation patterns affect the distribution of disease vectors, the survival of pathogens in the environment, and population vulnerability through food and water security impacts.
Prevention Strategies and Public Health Interventions
Effective prevention of the most dangerous diseases in today’s society requires comprehensive approaches that address individual behaviors, healthcare system capacity, and environmental factors. Vaccination programs represent one of the most successful public health interventions, with pneumococcal and influenza vaccines significantly reducing respiratory infection mortality in vulnerable populations.
Tobacco control measures demonstrate the potential for population-level interventions to achieve dramatic health improvements. Countries implementing comprehensive tobacco control programs, including taxation, advertising restrictions, and smoking bans, have achieved substantial reductions in smoking rates and associated disease burden.
Healthcare System Strengthening
Strong healthcare systems provide the foundation for effective disease prevention and treatment. Key components include trained healthcare workers, essential medicines, diagnostic capabilities, and referral systems. The COVID-19 pandemic highlighted both the importance of robust health systems and the vulnerabilities present in many countries’ healthcare infrastructure.
Primary healthcare serves as the cornerstone of effective health systems, providing accessible first-contact care and coordinating more specialized services when needed. Investment in primary healthcare yields significant returns, with every dollar invested generating economic returns of up to four dollars through improved health outcomes and productivity.
Community health worker programs have demonstrated effectiveness in extending healthcare reach to underserved populations. These programs train local community members to provide basic health services, health education, and connections to formal healthcare systems. Such approaches prove particularly valuable for managing chronic diseases and preventing infectious disease outbreaks.
Technological Innovations in Disease Management
Advances in medical technology continue to transform approaches to preventing and treating major causes of mortality. Artificial intelligence applications in medical imaging enable earlier detection of lung cancer and cardiovascular disease, potentially improving treatment outcomes through early intervention.
Telemedicine platforms expand access to specialized care, particularly valuable for populations in remote or underserved areas. These technologies proved essential during the COVID-19 pandemic and continue to evolve as permanent components of healthcare delivery systems.
Wearable devices and mobile health applications enable continuous monitoring of health parameters, empowering individuals to take active roles in managing their health. These tools show particular promise for managing chronic conditions such as COPD and heart disease, where early detection of changes in status can prevent hospitalizations.
Precision Medicine Approaches
The development of precision medicine approaches offers new hope for more effective treatment of complex diseases. Genetic testing can identify individuals at higher risk for certain conditions, enabling targeted prevention strategies. Pharmacogenomics helps optimize medication selection and dosing based on individual genetic profiles, potentially improving treatment effectiveness while reducing adverse effects.
Biomarker research continues to identify new ways to detect disease early and monitor treatment responses. These advances may lead to more personalized approaches to preventing and treating the major causes of global mortality.
Economic Implications of Global Health Threats
The economic burden of major health threats extends far beyond direct healthcare costs. Respiratory infections and cardiovascular diseases impose substantial costs through lost productivity, reduced economic growth, and increased social welfare needs. The World Bank estimates that health-related productivity losses cost the global economy trillions of dollars annually.
Individual families face devastating financial impacts from major health events. Medical expenses, combined with lost income due to illness or caregiving responsibilities, push millions of families into poverty each year. This economic impact creates cycles where poor health leads to poverty, which in turn increases health risks.
Healthcare systems face mounting pressure to provide effective care while controlling costs. The increasing prevalence of chronic diseases, aging populations, and rising healthcare costs create sustainability challenges for many health systems worldwide.
Future Challenges and Opportunities
Looking ahead, several trends will shape the landscape of global health threats. Population aging will increase the burden of chronic diseases, while urbanization may create new patterns of infectious disease transmission. Climate change will continue to influence disease patterns and healthcare system demands.
Antimicrobial resistance poses growing threats to the treatment of respiratory infections and other conditions. The development of new antibiotics has slowed dramatically, while resistance patterns continue to evolve. Addressing this challenge requires coordinated global action involving healthcare providers, researchers, policymakers, and the agricultural sector.
Emerging infectious diseases represent ongoing threats, as demonstrated by the COVID-19 pandemic. Strengthening global surveillance systems and pandemic preparedness remains crucial for detecting and responding to new health threats before they become global emergencies.
The Role of Global Cooperation
Addressing the world’s most dangerous diseases requires unprecedented levels of international cooperation. Infectious diseases cross borders freely, making national approaches insufficient. Climate change and air pollution represent global challenges requiring coordinated responses.
International organizations such as the World Health Organization play crucial roles in coordinating global health responses, setting standards, and providing technical assistance to countries with limited resources. However, political tensions and competing national interests sometimes limit the effectiveness of these efforts.
Conclusion: A Path Forward
The most dangerous diseases in today’s society—from lower respiratory tract infections to ischemic heart disease—represent complex challenges requiring comprehensive, sustained responses. While these conditions claim millions of lives annually, many deaths are preventable through known interventions including vaccination, tobacco control, air pollution reduction, and strengthened healthcare systems.
Success in addressing these challenges depends on sustained commitment from governments, healthcare systems, communities, and individuals. The tools and knowledge exist to significantly reduce the global burden of these diseases, but implementation requires political will, adequate resources, and coordinated action across sectors.
Individual actions matter significantly in this global effort. Personal choices regarding smoking cessation, physical activity, diet, and healthcare seeking behavior directly influence disease risks. Community engagement in prevention programs and advocacy for policy changes can drive population-level improvements in health outcomes.
For those seeking deeper understanding of these critical health challenges, comprehensive resources are available through our detailed analysis at Understanding Global Health Mortality, which provides additional insights into prevention strategies and emerging research in this vital field.
The path forward requires recognizing that health represents both a fundamental human right and a prerequisite for social and economic development. Investments in health systems, disease prevention, and health equity yield benefits that extend far beyond healthcare sectors, creating healthier, more prosperous societies for all. Through sustained commitment and coordinated action, the devastating impact of today’s most dangerous diseases can be substantially reduced, saving millions of lives and improving quality of life for countless more.
Leave a Reply