Table of Contents
Brainstem Origins
Intracranial Routes & Exit Foramina
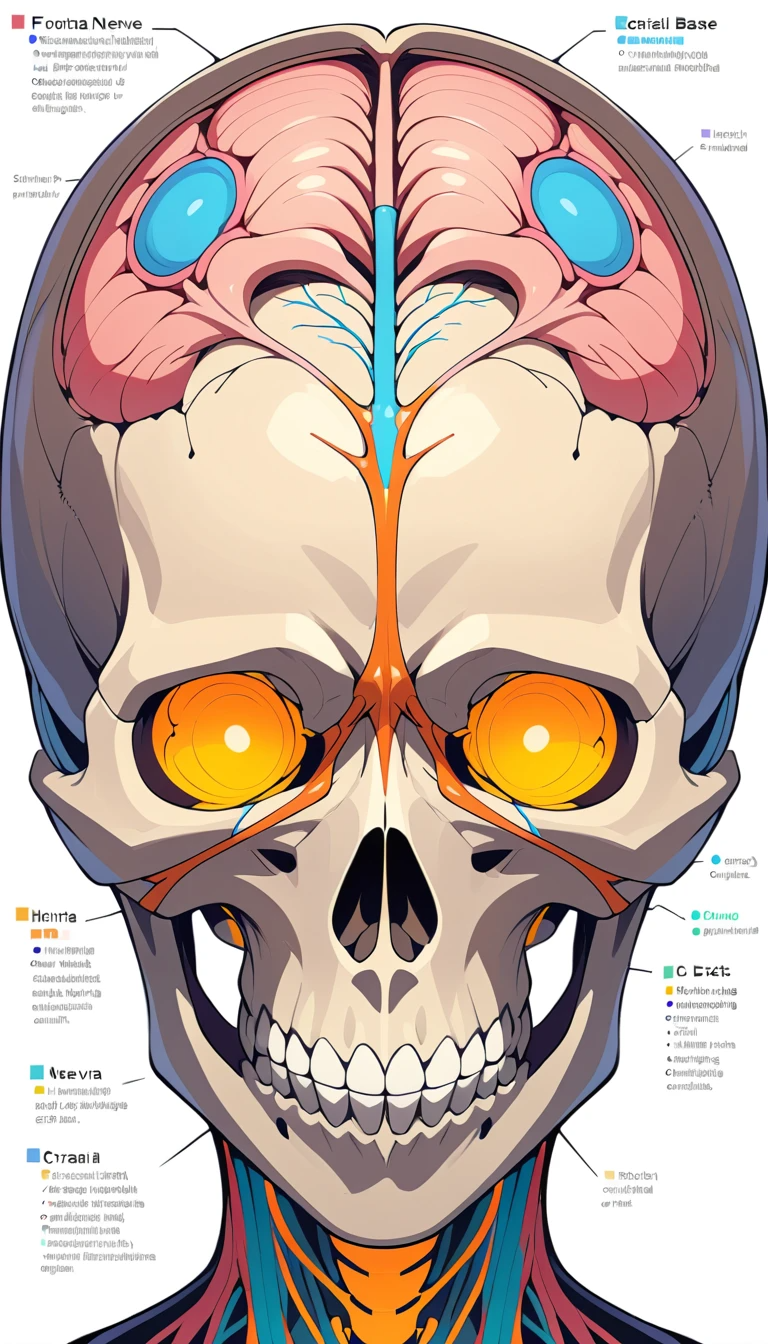
1. Overview of Cranial Nerves {#overview}
Cranial nerves are 12 paired nerves arising from the brain and brainstem. They conduct sensory, motor, or mixed signals—governing everything from smell to eye movement and facial expression. Understanding their function is vital across neurology, ENT, ophthalmology, and medical education.
According to Wikipedia, “Cranial nerves connect the brain to different parts of the head, neck, and trunk” and include special sensory fibers for smell, vision, taste, and hearing. These nerves exit the skull via specific foramina and track unique pathways.
2. Anatomy & Pathways {#anatomy-pathways}
Brainstem Origins
CN I (Olfactory) and CN II (Optic) originate from the cerebrum.
CN III–XII emerge from brainstem levels:
Midbrain: CN III, IV
Pons: CN V–VIII
Medulla: CN IX–XII
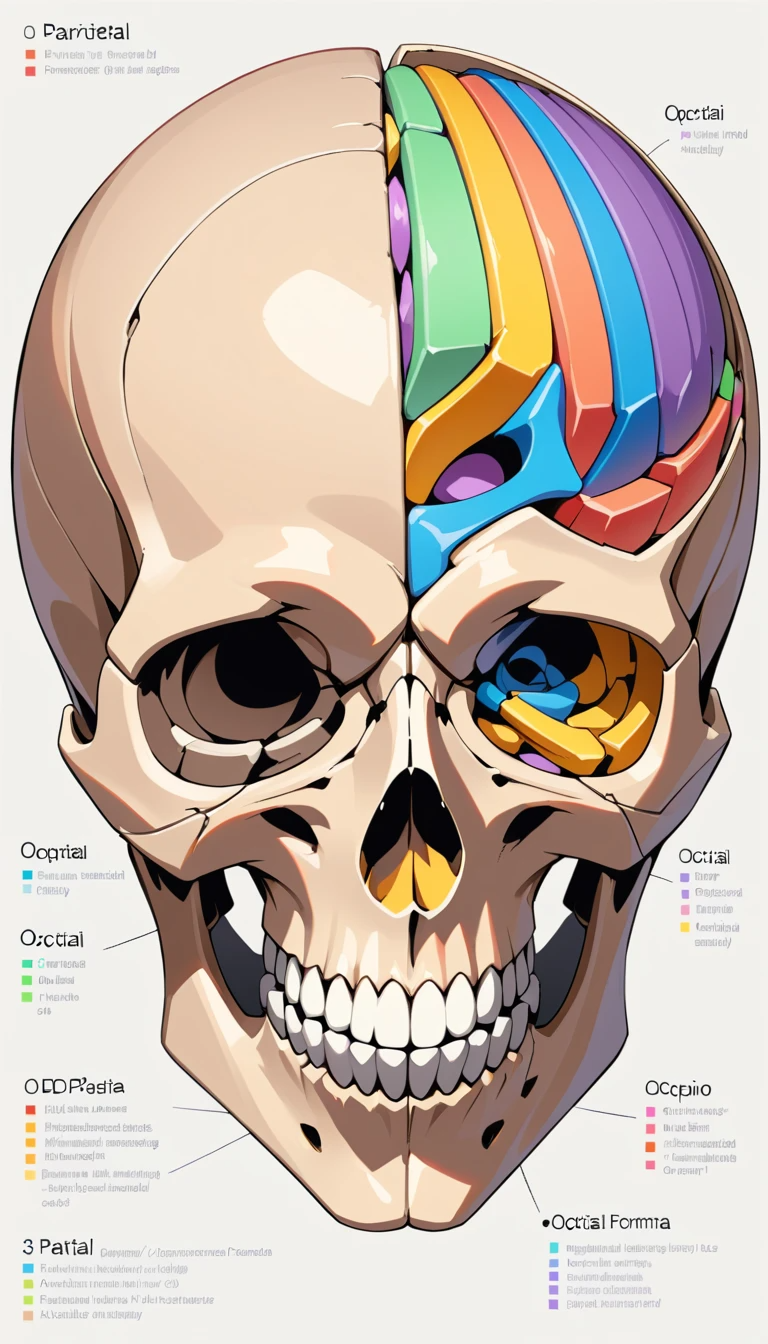
Intracranial Routes & Exit Foramina
Each nerve exits through skull openings:
CN I: cribriform plate
CN II: optic canal
CN III, IV, V1, VI: superior orbital fissure
CN V2: foramen rotundum
CN V3: foramen ovale
CN VII, VIII: internal acoustic meatus
CN IX, X, XI: jugular foramen
CN XII: hypoglossal canal
Don’t miss our guide on temporal bone anatomy for cross-referencing how CN VII–VIII travel near inner ear structures. Check it here: Temporal Bone Anatomy Deep Dive.


3. Individual Cranial Nerve Profiles (CN I–XII) {#profiles}
CN I – Olfactory
Function: Smell
Structure: Sensory fibers from the nasal epithelium to olfactory bulbs
Clinical Highlight: Unique ability to regenerate—research explores olfactory nerve regeneration for neurodegenerative disease assessments.
CN II – Optic
Function: Vision, pupillary reflex
Route: Retina → optic canal → optic chiasm
Common Issues: Glaucoma, optic neuritis, papilledema
CN III – Oculomotor
Function: Raises eyelid, moves most extraocular muscles, pupillary constriction
Exam Note: Look for droopy eyelid (ptosis), “down and out” eye, and pupil involvement.
CN IV – Trochlear
Function: Moves superior oblique (downward inward gaze)
Clinical Case: Trochlear palsy can result in vertical diplopia—worsens when looking down.
CN V – Trigeminal
Projections:
V1 – upper face sensation
V2 – mid-face sensation
V3 – jaw motor control
Disorders: Trigeminal neuralgia—sudden severe facial pain; often treated with anticonvulsants (carbamazepine)
CN VI – Abducens
Function: Abducts the eye (lateral movement)
Weakness: Medial horizontal diplopia; could signal raised intracranial pressure (false localizing sign).
CN VII – Facial
Role: Facial expression, taste (anterior 2/3 tongue), lacrimation, salivation
Common Disorder: Bell’s palsy – peripheral facial paralysis; treatable with corticosteroids.
CN VIII – Vestibulocochlear
Function: Hearing + balance
Disorders: Vestibular neuritis, Ménière’s disease—check Wikipedia for full overview.
CN IX – Glossopharyngeal
Functions: Taste (posterior tongue), swallow, carotid body reflex
Clinical Tip: Rare glossopharyngeal neuralgia may mimic ear pain and require surgical options.
CN X – Vagus
Functions: Voice, swallowing, parasympathetic control of heart and gut
Systems Impacted: GI motility, cardiac rate, laryngeal muscles
CN XI – Accessory
Function: Trapezius & sternocleidomastoid—shoulder elevation and head rotation.
CN XII – Hypoglossal
Role: Tongue movement
Injury Signs: Tongue deviation toward affected side; slurred speech.
4. Modalities & Functions {#modalities}
| Type | Nerves (I–XII) |
|---|---|
| Sensory Only | I, II, VIII |
| Motor Only | III, IV, VI, XI, XII |
| Mixed | V, VII, IX, X |
Subtypes include:
Special somatic (vision, hearing)
General visceral (parasympathetic via vagus)
General somatic (muscle movement)
General visceral sensory (taste, baroreception)
5. Common Disorders & Clinical Cases {#disorders}
Ocular Motor Palsies (III, IV, VI) — may signal microvascular ischemia or nerve compression
Facial Nerve Palsy (VII) — idiopathic or due to Lyme disease/HSV
Trigeminal Neuralgia — shock-like facial pain; often treated with medications and sometimes microvascular decompression
Glossopharyngeal Neuralgia — throat/ear pain; rare but disabling
Optic Neuritis — sudden vision loss
Vestibular Disorders — dizziness, tinnitus, hearing loss
Vagus Dysfunction — gastroparesis, fainting spells, vocal cord weakness
6. Diagnostic Tests & Assessment {#diagnosis}
Clinical exam: Follow each nerve with sensory testing, strength tests, reflexes, eye tracking, tongue movement.
Imaging: MRI/CT scans—especially for exit foramina or temporal bone areas where CN VII/VIII travel. Our temporal bone anatomy guide helps interpret such images.
Electrophysiology: EMG and nerve conduction studies—essential for differentiating central vs peripheral palsies.
7. Treatment & Management {#treatment}
Preventive health: Maintain healthy blood pressure, manage diabetes, avoid head trauma.
Bell’s palsy: Start corticosteroids early.
Neuralgias: Use anticonvulsants (e.g., carbamazepine, gabapentin), and consider surgery if refractory.
Ocular palsies: Eye patches, corrective prisms, surgery for alignment.
Vagus issues: Treat GI motility problems, manage voice/swallowing deficits, consider pacemaker for syncope.
8. Memory Aids & Mnemonics {#mnemonics}
Nerve Names: “On Old Olympus’ Towering Tops, A Friendly Viking Grew Vines And Hops” (CN I–XII)
Types Mnemonic: “Some Say Marry Money, But My Brother Says Big Brains Matter Most”
Foramina Chart: Print out a diagram listing each nerve with its exit point
Clinical Case Mnemonics:
Trochlear palsy: “When reading on the stairs, the steps double”—focuses on vertical diplopia when looking down.
9. Conclusion {#conclusion}
Cranial nerves are the highway between your brain and head/neck functions. Recognizing their anatomy, including brainstem origins and skull exit routes, is critical for accurate diagnosis and treatment. Incorporating functional mnemonics boosts retention, and deeper learning—like the paths of CN VII/VIII through the temporal bone—ties right into places like our temporal bone anatomy post.
For authoritative background, check:
Wikipedia’s Cranial Nerves page for detailed definitions
Cleveland Clinic for clinical treatment options, especially on trigeminal neuralgia and facial palsy
Forbes Health for layperson-friendly articles on nerve function and health
By combining clarity, authority, and clinical relevance, this guide offers deep yet accessible insights into cranial nerve anatomy and pathology—designed to boost your blog’s SEO impact and engage readers seeking trustworthy medical knowledge.
Leave a Reply